Knowing your results helps you and your doctor understand what’s best for your health. Results are usually ready in 7-10 days.
Make the most of your Medicare. Sign up to get important reminders & information about Medicare and COVID-19. The terms 'HCA' or the 'Company' as used in this website refer to HCA Healthcare, Inc. And its affiliates, unless otherwise stated or indicated by context. The term 'facilities' refers to entities owned or operated by subsidiaries or affiliates of HCA Healthcare, Inc. References herein to 'HCA employees' or to 'our employees' refer to employees. Healthvana is a HIPAA-secure, mobile-friendly portal for patients to manage their health. We’ve partnered with COVID-19 testing locations to help deliver test results, education, and other relevant information.

You can now view MyQuest™ results in the Apple Health app.* This allows you to easily and securely view your lab results in the same place as your other important health data.
See steps on how to add Quest Diagnostics to your health records.
Two ways to get your lab results
Directly through MyQuest™
|
From your doctor's office |
After you have your results
In either case, it's important to discuss your results with your doctor. Together, you two can decide what’s best for your health.
Next steps
Download the App now
We do not charge a fee to use this app. However, your carrier’s data and usage charges apply.
For Apple® iPhone, iPod Touch, iPad, Android™

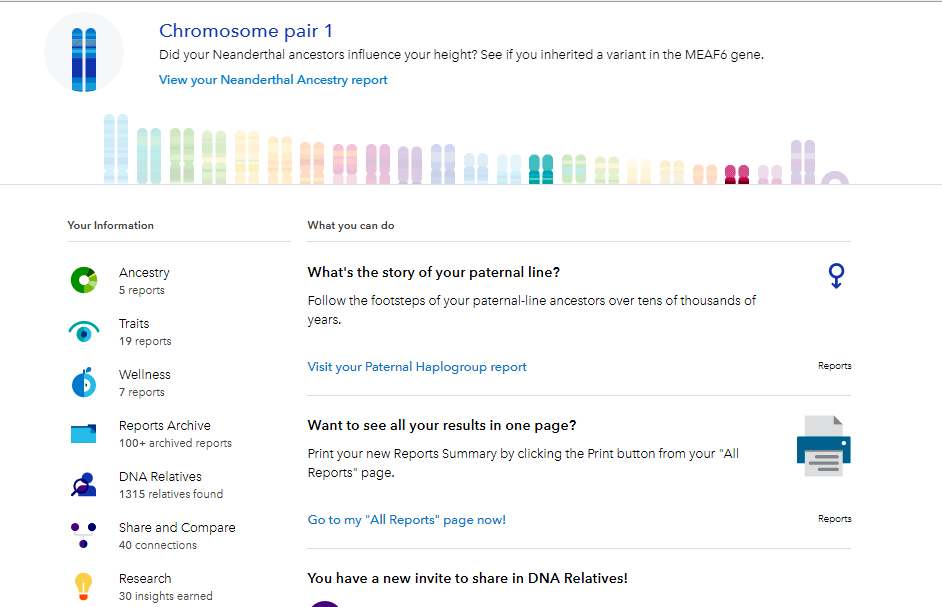
*Available on iPhones running IOS 11.3 or later.
The coronavirus pandemic has resulted in millions of cases across the globe. The United States has one of the highest death rates due to COVID-19 across the world, and its mortality rates will likely increase. Due to different approaches to containing the virus across countries – as well as the quality and accessibility of health care – we may see diverging rates of mortality, disease burden, and other measures of health outcomes between the U.S. and comparable countries. This chart collection provides a baseline of how the U.S. already compared to similarly large and wealthy countries prior to the onset of the coronavirus pandemic.
The following charts and a related brief explore a number of different metrics used to look at health outcomes, quality of care, and access to services. While inconsistent and imperfect metrics make it difficult to firmly assess system-wide health quality in the U.S., a review of the available data prior to the onset of the pandemic suggests that in most of these measures, the U.S. continued to lag behind comparably wealthy and sizable countries. As rates of all-cause mortality, maternal mortality, and years of life lost have stagnated or increased over time, the gap has widened between the U.S. health system and those of its peers.
We examine long-term outcomes, treatment outcomes, hospital-related care and patient safety in the U.S. and 11 other countries identified as similarly wealthy based on GDP and GDP per capita. The data from most of the charts come from the Organization for Economic Co-operation and Development (OECD), which has compiled health quality statistics and data from several countries around the world. It is important to note that the healthcare systems, populations, and public health responses in these countries can vary considerably, and that these factors play a role in population health outcomes.
All-cause mortality rates have fallen steadily in the U.S. and in comparable countries
One method for measuring quality is to look at all-cause mortality rates (number of deaths per 100,000 people, adjusted for age differences across countries). Mortality rates are influenced by a myriad of factors, including the quality and availability of healthcare. The mortality rate has been falling in the U.S. and in comparable countries. From 1980 to 2017, the overall mortality rate for all causes of death in the U.S. fell about 29%, compared to a 44% decline in comparable countries. The gap in mortality rates may shift after accounting for COVID-19 related deaths, since the U.S. currently leads in the number of deaths due to COVID-19 and its mortality rate is likely to increase.
The mortality rate for respiratory diseases is higher in the U.S. than in comparably wealthy countries
Mortality rates for respiratory diseases fell over the last 10 years in the U.S. and across comparable countries. However, from 1980 to 2017, the U.S. mortality rate for respiratory diseases increased by nearly 5%, while comparable countries experienced a 36% decline.
These rates are prior to accounting for deaths from COVID-19. Since COVID-19 is a respiratory disease, rates of mortality due to respiratory diseases in particular may increase because of the pandemic.
In 2017, 278,673 people died due to diseases of the respiratory system in the U.S. As of August 19, 2020, over 172,000 individuals died due to COVID-19 in the U.S.
Mortality rates for diseases of the circulatory system have fallen dramatically over the last 37 years
The U.S. and other countries have made dramatic progress in lowering mortality from diseases of the circulatory system. In the U.S., the mortality rate has fallen from 629 deaths per 100,000 population in 1980 to 255 in 2017; deaths due to diseases of the circulatory system also accounted for a smaller share of all-cause mortality in 2017 (30%) than they did in 1980 (53%). Although the U.S. mortality rate for diseases of the circulatory system has improved by 59%, similar countries have seen an average improvement of 65% over the same time period, from 607 deaths per 100,000 to 210, on average. In recent years, this decline has reversed course, and the number of deaths due to diseases of the circulatory system have started slowly increasing. In 2017, 859,098 people died due to diseases of the circulatory system in the U.S.
The mortality rate for cancers has been falling in the U.S. and across comparable countries
While there is debate over the best way to measure outcomes for cancer, the U.S. has performed better than peer countries with lower rates of death due to cancer over the past 15 years. Overall, the mortality rate for all cancers has fallen steadily in the U.S. and in comparable countries over the last 37 years. In the U.S., the age-adjusted mortality rate for cancers fell 24% from about 242 deaths per 100,000 population in 1980 to about 183 per 100,000 in 2017. The comparable country average fell 26% over the same period, from 262 deaths per 100,000 to 198. In 2017, the number of people who died in the U.S. due to cancer was 614,988.
After a steady decline in premature death rates, the U.S. has experienced a recent uptick
An alternative to overall mortality rates is “years of life lost”, a marker of premature deaths. Years of life lost is measured by adding the collective years lost by those in a population who died before a specified age (e.g. 70). For example, a person who dies at age 45 would have 25 years of life lost. As a measure, it provides more weights to deaths at younger ages. The U.S. and comparable OECD countries have made progress in reducing years of life lost over the last 27 years (down 23% and 42%, respectively), although the gap between the U.S. and comparable countries increased over to time, standing at 12,282 vs. 7,780 years of life lost in 2017. It remains to be seen how this measure is influenced by the impact of COVID-19 on individuals who survive the disease.
Disease burden is higher in the U.S. than in comparable countries
Disease burden, which accounts for both premature death and years living with disability, is often measured using disability adjusted life years (DALYs). Though DALYs have declined in the U.S. and comparable countries since 2000, the U.S. continues to have higher age-adjusted rates than those of peer countries. In 2017, the DALYs rate was 31% higher in the U.S. than for comparable countries, on average.
The U.S. ranks last in a measure of health care access and quality, indicating higher rates of amenable mortality than peer countries
Mortality amenable to healthcare is a measure of the rates of death considered preventable by timely and effective care. While the health care system might not be expected to prevent death in all instances, differences in amendable mortality indicate how effectively healthcare is delivered. The Healthcare Access and Quality (HAQ) Index is scaled from 0 (worst) t0 100 (best) and is based on amenable mortality. The HAQ index uses age-standardized, risk-standardized mortality rates for 32 causes of death that timely and effective health care could potentially prevent. Lower scores indicate high mortality rates for causes amenable to health care, while higher scores indicate lower mortality rates, possibly reflecting better quality and access to care. The U.S. ranks last among comparable countries on the HAQ index with a score of 88.7.
Maternal mortality rates in the U.S. have risen over time and are much higher than in peer countries
While wealth and economic prosperity are highly correlated with lower maternal mortality rates, the U.S. is an outlier with the highest rate of pregnancy-related deaths (16.9 deaths per 100,000 live births) when compared to similar countries (4.4 deaths per 100,000 live births).
As the gulf continues to widen, the data points towards significant racial and geographic disparities in maternal mortality in the U.S., with Black women more than three times as likely to die from pregnancy-related causes compared to White women and mortality ranging widely between different states.
30-day mortality for heart attacks and strokes is lower in the U.S. than in comparable countries
Mortality within 30 days of being admitted to a hospital is not entirely preventable, but can be reduced for certain diagnoses and services. Improvement in this area is often linked to improved quality of care. The 30-day mortality rates after hospital admissions for heart attacks (acute myocardial infarction) and hemorrhagic stroke (caused by bleeding) are similar in the U.S. and comparable countries. The 30-day mortality rates for ischemic strokes (caused by blood clots) is 4.2 deaths per 100 patients in the U.S., compared to an average of 7.0 deaths per 100 patients in similar countries.
Hospital admissions for chronic conditions that are risk factors for COVID-19 are more frequent in the U.S. than in comparable countries
Hospital admissions for certain chronic diseases like circulatory conditions, chronic obstructive pulmonary diseases (COPD), asthma, and diabetes, can arise for a variety of reasons, but preventative services – or lack thereof – play a large role. Hospital admission rates in the U.S. are higher than in comparable countries for congestive heart failure, COPD, asthma, and complications due to diabetes. Hospital admissions for these chronic conditions could be minimized with adequate primary care.
The rates for hospitalization for such chronic conditions may change during the pandemic. Reports suggest hospitalizations for non-COVID-19 related conditions decreased in the first few months of the pandemic, particularly in hard-hit regions of the U.S. to create greater capacity to treat COVID-19. To the extent patients delay getting needed care, disease burden and hospitalizations could increase in the longer run.
More cesarean sections are performed in the U.S. than in comparable countries
Cesarean sections are the most commonly performed surgical procedures in the U.S. and have become a key indicator of quality of care in maternal health. Cesarean sections can be lifesaving; however, when they are not medically indicated, they can pose unnecessary risks for both the mother and newborn, including an increased chance of blood clots, infections, and other complications that require further surgery.
The U.S. has consistently had higher cesarean section rates than its peers, on average, though rates have decreased slightly in recent years. In 2015, the rate of cesarean sections per 1,000 live births with inpatient admissions was 320 in the U.S. and 269 in comparable countries.
Obstetric trauma during vaginal delivery is more common in the U.S. than some comparable countries, especially when instruments are involved
Obstetric trauma is more likely to occur in deliveries where instruments are utilized (i.e. forceps). The rate of obstetric trauma during deliveries with an instrument in the U.S. was 11.1 per 100 vaginal deliveries in 2016, higher than most comparable countries with available data. The rate of obstetric trauma during deliveries without an instrument in the U.S. was 1.7 per 100 vaginal deliveries in 2016, slightly lower than most other comparable countries with available data.
Post-operative clots are more common in the U.S. than in some comparable countries
Rates of post-operative complications are an important measure of hospital-based safety. Pulmonary embolisms and deep vein thrombosis are common complications after major surgeries, such as hip or knee replacement. The prevalence of post-operative clots for these procedures is higher in U.S. than in Germany, the U.K., and Sweden (comparable countries with recent data).
Post-operative sepsis is less common in the U.S. than in some peer countries

Sepsis is a spectrum of disease afflicting patients with infections, that can range from organ failure and shock to death in severe cases. Rates of post-operative infections and sepsis is an important marker of quality in patients undergoing surgery because this is a major source of morbidity and mortality and can sometimes be prevented. Prevention is multifactorial and can be affected by operative techniques and training, hygiene and safety protocols and antibiotic utilization amongst other things. The rate of post-operative sepsis following abdominal surgery is just above 1% in the U.S., slightly lower than in most other countries that report data, with the exception of Canada.
The U.S. has higher rates of medical, medication, and lab errors than comparable countries
Patients in the U.S. are more likely than those in comparable countries to experience a medical error at some point during their care, according to a survey by the Commonwealth Fund. In this case, medical errors include being given the wrong medication or dose or experiencing delays or errors in laboratory test results. In 2016, 19% of patients in the U.S. experienced a medical error compared to 12% of patients in similar countries.
Somos Health Care
The authors would like to thank Dustin Cotliar, MD, MPH for his contributions.